A groundbreaking study published in Nature Mental Health has uncovered a potential connection between gut microbiota and depression, offering new hope for treatment-resistant cases. Researchers found that individuals with major depressive disorder (MDD) often exhibit distinct imbalances in their gut bacteria compared to those without the condition. This discovery opens the door to innovative therapies targeting the gut-brain axis, a complex communication network linking the digestive system and emotional regulation.
The human gut hosts trillions of microorganisms, collectively known as the microbiome, which play a crucial role in digestion, immunity, and even neurotransmitter production. Scientists have long suspected that disruptions in this delicate ecosystem could influence mental health, but only recently has technology advanced enough to explore this relationship in depth. The study analyzed stool samples from over 1,000 participants, half of whom had been diagnosed with depression. The results revealed significant differences in microbial diversity, with depressed individuals showing lower levels of beneficial bacteria such as Bifidobacterium and Lactobacillus.
Further experiments in mice supported these findings. When researchers transplanted gut bacteria from depressed humans into germ-free mice, the animals began displaying behaviors associated with depression, such as reduced mobility and lack of interest in pleasurable activities. Conversely, mice given probiotics or dietary changes aimed at restoring microbial balance showed marked improvements in mood-related behaviors.
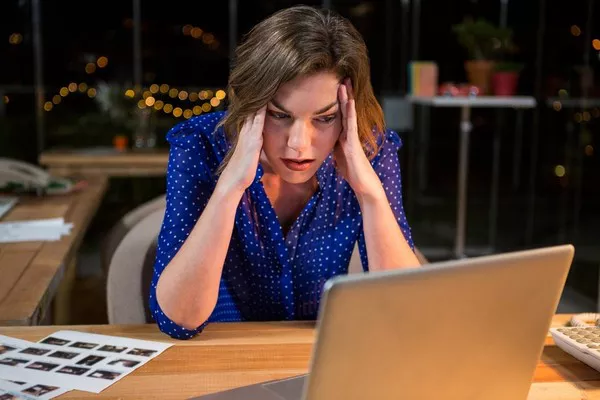
These findings could revolutionize depression treatment. Current antidepressants, which target serotonin and other neurotransmitters, are ineffective for nearly 30% of patients. If gut bacteria influence mental health, therapies like probiotics, prebiotics, or even fecal microbiota transplants (FMT) could provide alternative or complementary solutions. Early clinical trials have shown promise—a pilot study reported that participants who took a specific probiotic strain for eight weeks experienced a significant reduction in depressive symptoms compared to a placebo group.
However, experts caution that more research is needed before these treatments become mainstream. The gut-brain connection is highly complex, and individual variations in microbiome composition mean that a one-size-fits-all approach may not work. Additionally, long-term safety and efficacy must be thoroughly evaluated.
Despite these challenges, the study represents a major step forward in understanding depression’s biological underpinnings. It also highlights the importance of holistic health approaches, emphasizing diet, exercise, and gut health as potential tools in mental wellness. As research progresses, the hope is that these discoveries will lead to more effective, personalized treatments for those suffering from this debilitating condition.
Related topics: