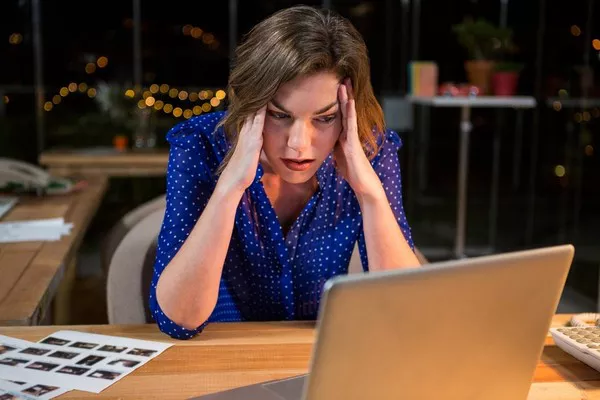
A landmark study published in Nature Neuroscience has demonstrated unprecedented success in treating severe depression using precisely targeted magnetic stimulation to rebuild neural connections. The Stanford-led research team developed a new form of repetitive transcranial magnetic stimulation (rTMS) that combines functional MRI guidance with real-time neural feedback, allowing clinicians to identify and stimulate specific atrophied pathways in the prefrontal cortex. In the clinical trial involving 278 treatment-resistant patients, 63% achieved full remission after just four weeks of treatment—double the effectiveness of traditional rTMS protocols.
What sets this approach apart is its personalized precision. Using machine learning algorithms trained on thousands of brain scans, the system creates individualized stimulation maps based on each patient’s unique neural architecture. Dr. Ethan Zhou, the study’s lead researcher, explains: “We’re not just stimulating random areas—we’re identifying the exact communication breakdowns in each person’s mood regulation network and rebuilding those pathways.” The treatment appears to trigger a cascade of neuroplastic changes, with patients showing measurable increases in gray matter density after treatment that correlate with symptom improvement.
The implications extend beyond depression. Early trials for PTSD show similar neural pathway restoration, and researchers are optimistic about applications for anxiety disorders and even some forms of dementia. While currently expensive due to the advanced imaging required, several biotech firms are racing to develop more accessible versions of the technology. As this treatment moves toward FDA approval, it represents a paradigm shift from managing symptoms to actually repairing the underlying neurological damage caused by mental illness.
Related topics: