A new form of non-invasive brain stimulation is showing unprecedented results in treating severe obsessive-compulsive disorder (OCD) that doesn’t respond to traditional therapies. The technique, called deep transcranial magnetic stimulation (dTMS), uses magnetic fields to target and normalize activity in the hyperactive brain circuits associated with OCD.
In a landmark multi-center trial published in the American Journal of Psychiatry, 70% of participants experienced significant symptom reduction after six weeks of treatment, with benefits lasting at least six months.
The treatment focuses on modulating activity in the cortico-striato-thalamo-cortical (CSTC) loop, the neural pathway that becomes stuck in repetitive loops in OCD patients. Unlike traditional TMS used for depression, the OCD protocol requires a specialized “H-coil” that reaches deeper brain structures. Patients undergo daily 20-minute sessions while awake, experiencing only mild tingling sensations. “It’s like hitting the reset button on malfunctioning brain circuits,” explains Dr. Rachel Levin, lead researcher at UCLA’s OCD program.
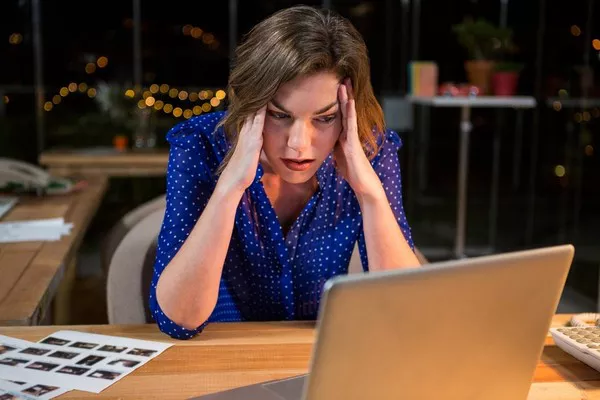
One trial participant, 34-year-old graphic designer Mark T., had suffered from debilitating contamination fears that required 4-hour showering rituals. “After three weeks of dTMS, I noticed the compulsive urges fading. For the first time in 15 years, I could touch a doorknob without panicking.” Functional MRI scans confirmed measurable changes in his brain activity patterns corresponding with symptom improvement.
While not a cure, dTMS offers hope for the estimated 30% of OCD patients who don’t respond to medications or cognitive behavioral therapy. The FDA approved the treatment in 2018, but insurance coverage remains limited. At $10,000-$15,000 for a full course, cost remains a significant barrier. Researchers are now investigating whether combining dTMS with traditional therapies could boost effectiveness further. “This represents a paradigm shift in how we approach treatment-resistant OCD,” says Levin. “We’re finally able to directly address the neurological roots of the disorder.”
Related topics: